Understanding Anatomophysiology and Cardiovascular Diseases
Cardiovascular diseases are the leading cause of death worldwide. According to the World Health Organization, these diseases claimed 17.9 million lives in 2019, which represents 32% of all global deaths. Heart attacks and strokes accounted for 85% of these, signaling a significant global health issue. This post delves into the complexities of these conditions, emphasizing the importance of awareness. We explore the anatomy and physiology of the circulatory and cardiovascular systems, discuss common symptoms, and identify risk factors. Our goal is to increase awareness to promote prevention, early detection, and better management of cardiovascular health.
To understand the causes of cardiovascular diseases (CVDs), it's crucial to grasp the anatomy and physiology of the circulatory and cardiovascular systems. Especially, understanding the functions of the heart and blood vessels offers valuable insights into the factors contributing to the onset and progression of CVDs.
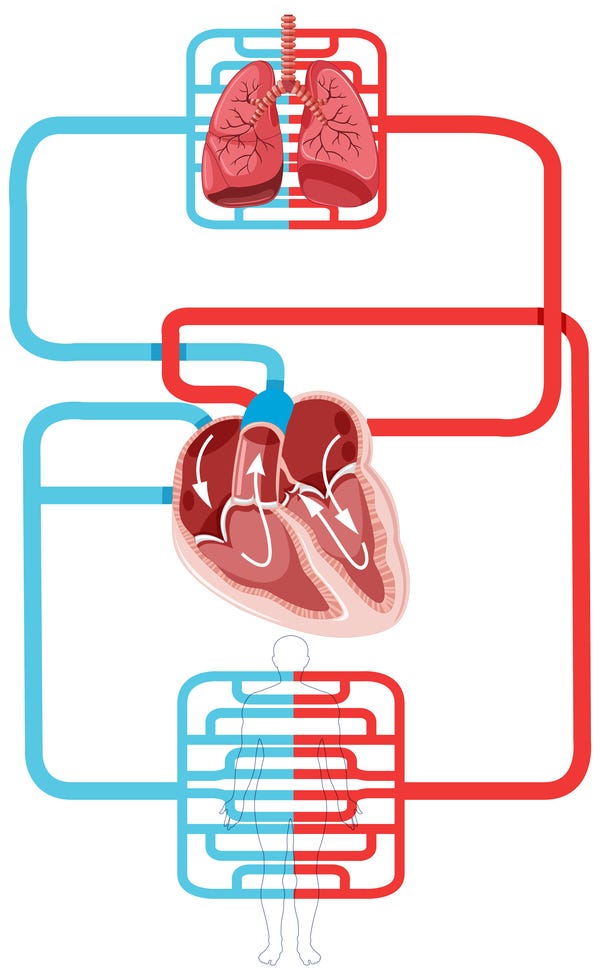
The circulatory system, a closed network of vessels, connects the systemic and pulmonary circulations through the heart. The systemic circulation starts with the aorta artery, which branches into several channels to supply blood to various organs and body areas. After traveling through the systemic circulation, the blood reaches the right atrium via the superior and inferior vena cava, marking the end of the cycle. The right ventricle then pumps this deoxygenated blood into the pulmonary circulation for gas exchange, where it releases carbon dioxide (CO2) and absorbs oxygen (O2). The oxygen-rich blood returns to the heart through four pulmonary veins and enters the left atrium.
Blood pressure maintains blood flow within vessels via systemic circulation. Arterioles, smaller arteries located within organs, offer resistance to blood flow and regulate blood pressure through internal processes like hormones, chemicals, and neurons. Vasodilation, the widening of the vessel, reduces blood pressure, while vasoconstriction, the narrowing of the vessel, increases it. This mechanism allows for the delivery of more nutrients and oxygen to tissues during periods of high metabolic demand, such as during exercise. Capillaries—thin-walled tubes enabling gas exchange between blood and tissues—represent the endpoint of systemic circulation. Veins then transport the blood back to the heart, aided by venous valves that prevent backflow and offset gravity's influence on blood circulation (Figure 2).
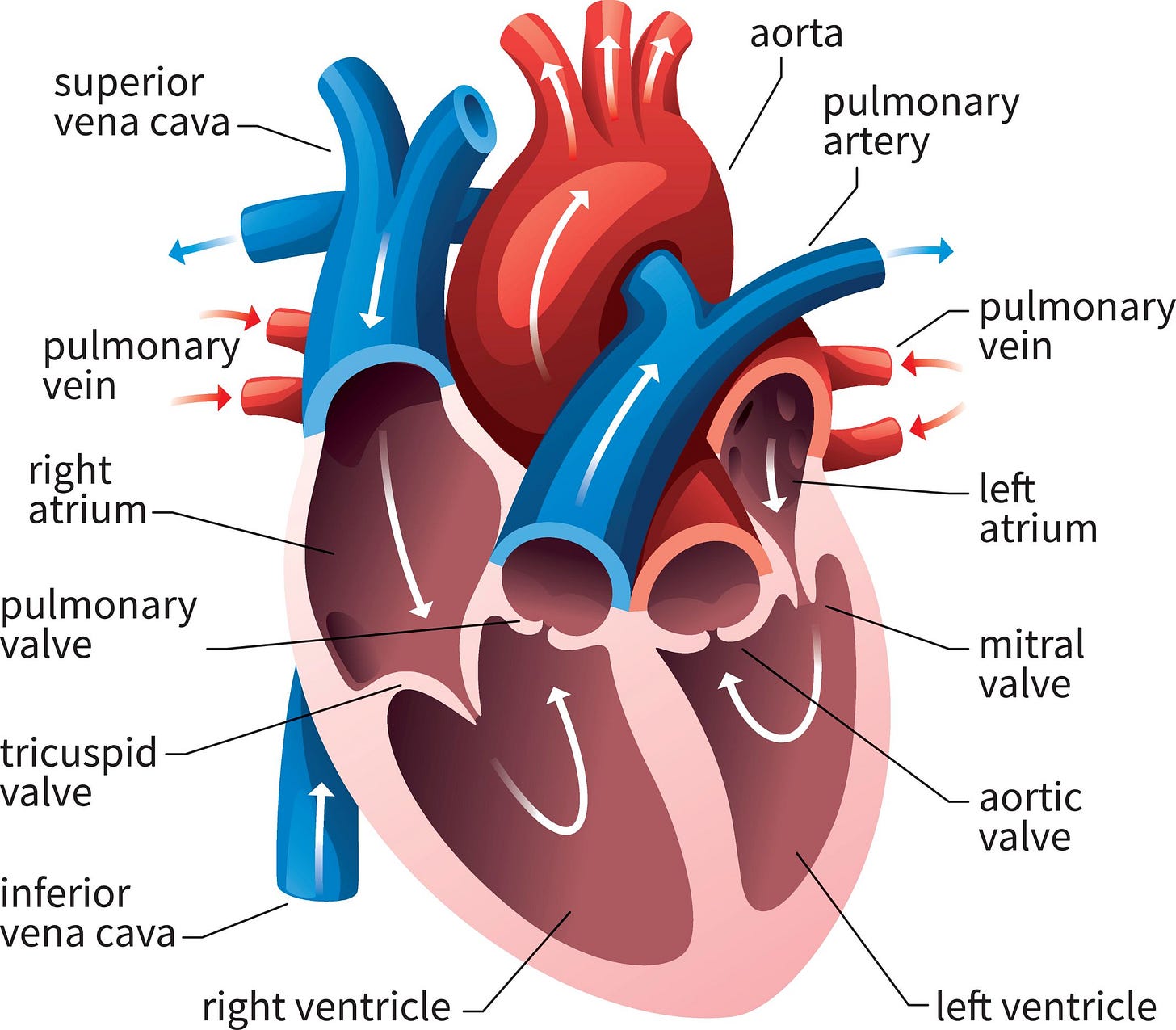
The heart is situated in the thoracic cavity between the lungs slightly off-center, with a majority of it lying to the left of the midline in the chest. Its outer layer, the pericardium, is composed of several membrane layers. The heart's four internal chambers consist of the lower right and left ventricles, and the upper right and left atria. Under normal circumstances, blood does not flow between the right and left chambers of the heart. The atria receive venous blood, with the left atrium receiving it from the body and the right from the lungs. The ventricles pump blood throughout the body, with the left ventricle being noticeably thicker owing to its role in systemic circulation and high-pressure pumping (Figure 3).
The myocardium, located near the heart's apex, functions as its "engine". Composed of cardiac muscle cells, it contracts in response to electrical signals triggered by action potentials. This allows the heart to pump blood rhythmically and automatically.
Despite these complex and millimetrically organised systems, cardiovascular diseases (CVDs) are prevalent and the leading cause of death globally. CVDs encompass conditions affecting the veins, arteries, and heart wall. Individuals with CVDs may be symptomatic (displaying physical symptoms) or asymptomatic (without noticeable symptoms). Symptoms can be classified into two groups: those related to blood vessels (such as veins and arteries) and those related to the heart itself.
Blood vessel symptoms, potentially noticeable throughout the body, include pain or cramping while exercising, non-healing sores on the legs, changes in skin temperature like coolness or redness in the legs, leg swelling, facial or limb numbness (often affecting only one side of the body), and difficulties with speech, vision, or walking.
Heart-related symptoms can include angina, which is intermittent chest pain, sensations of pressure or discomfort in the chest, shortness of breath, dizziness, fainting, and extreme fatigue.
Common blood vessel diseases may involve peripheral artery disease, which is the narrowing or blockage of arteries, cerebrovascular disease, aortic complications, deep vein thrombosis, and more. However, the most frequently seen cardiovascular diseases (CVDs) affect the heart. These include arrhythmias, or abnormal electrical conduction, heart valve issues, heart failure, and congenital heart defects present at birth, among others.
Certain risk factors (Figure 4) can increase the chances of developing cardiovascular disease. These include high blood pressure, high cholesterol levels, smoking, type 2 diabetes, a family history of heart disease, a sedentary lifestyle, being overweight or obese, a diet rich in fat, sugar, and sodium, excessive alcohol use, and misuse of prescription or recreational drugs.
Neglected cardiovascular diseases (CVDs) can lead to severe medical issues like heart attacks, strokes, and acute limb ischemia. However, routine screenings can detect these diseases early, enabling patients to live fulfilling lives while effectively managing their cardiovascular health under professional care. Prevention methods include regular check-ups and lifestyle modifications that reduce risk factors, such as adopting a balanced diet, maintaining regular exercise, managing stress effectively, and addressing any existing health conditions.
In short, understanding CVDs is crucial to mitigate their global health impact. Given the complexity of these diseases and the cardiovascular system, early detection and proactive treatment are vital to minimize their repercussions. By raising awareness, educating others, and adopting healthier lifestyles – including regular exercise, balanced diet, and stress management - individuals can reduce risk factors and enhance cardiovascular outcomes. Stay tuned for our forthcoming articles, where we'll delve into specific cardiovascular disorders and explore effective management strategies, empowering people to take charge of their cardiovascular health and well-being.
References:
Clinic, C. (2022). Cardiovascular Disease: Types, Causes & Symptoms. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/21493-cardiovascular-disease
World. (2021, June 11). Cardiovascular diseases (CVDs). Who.int; World Health Organization: WHO. https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
Silva, M. E. (2019). Sistemas Orgânicos Internos. Lisboa: FMH Edições. Capítulo 8.